
1787: The University of Pittsburgh, originally named the Pittsburgh Academy, is founded.
1886: The Western Pennsylvania Medical College is formed by local physicians, then acquired by the University of Pittsburgh just over 20 years later.
1942: Western State Psychiatric Hospital is established with a capacity of 200 beds, an outpatient clinic, a research center, and training programs for medical and nursing students.
1945-46: The newly renamed Western State Psychiatric Institute and Clinic begins a residency program in psychiatry and establishes a Department of Research.
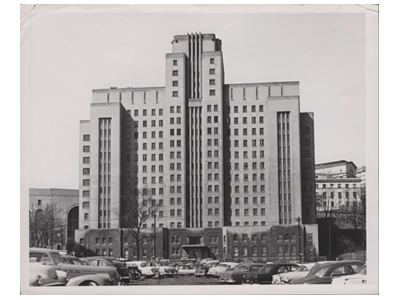
Western Psychiatric Institute and Clinic, 1955 1949: Pennsylvania transfers the management of the Western State Psychiatric Institute and Clinic to the University of Pittsburgh. It is again renamed, becoming the Western Psychiatric Institute and Clinic (WPIC).
1973: Thomas Detre, MD, is recruited from Yale University to lead the Department and WPIC. From Yale, Dr. Detre brings colleagues including Loren Roth, MD and David Kupfer, MD.
1983: Dr. Kupfer is named Chair, Department of Psychiatry, as Dr. Detre is appointed Vice Chancellor for Health Sciences; from this position, Dr. Detre later forms UPMC. Dr. Kupfer promotes collaborations between clinical investigators in psychiatry and those in neuroscience and other basic sciences. WPIC becomes one of the nation’s largest university-based clinical, educational, and research facilities.
1987: David Lewis, MD, joins the Department as Associate Professor of Psychiatry and Neuroscience and serves as Director of Basic Research for the Department.
2000: Dr. Lewis establishes the Translational Neuroscience Program (TNP), focused on understanding the neurobiological basis for human cognitive and emotional functions and how disturbances in these functions arise from alterations in the brain.
2009: Dr. Lewis is appointed Chair, Department of Psychiatry, and Medical Director & Director of Research, WPIC.

David Lewis, MD
As Chair, Dr. Lewis has prioritized building a faculty composed of individuals who bring innovative and creative approaches to scientific research, clinical care and medical and scientific training. He has also prioritized cultivating a multi-faceted academic community that thrives on collaboration across disciplines and roles.
Central to these priorities is a commitment to recruiting talented early-career investigators and clinician-educators who contribute fresh perspectives and actively engage in the department’s collaborative culture.
Pursuit of these priorities has been the development of many new initiatives that strengthen career development pathways with programs tailored to the specific needs of clinician-educators and investigators.
Clinical Trainees
2009-2010: The Department establishes a mentorship program for all residents, and substantially revamps Academic Administrator Clinician Educator (AACE) Track.
2013: The revised and renamed Psychiatry Research Pathway provides mentorship and other scientific career development resources for residents with a passion for research.
2014: Pitt Psychiatry initiates the Psychosomatic Clinical Fellowship (now known as the Consultation-Liaison in Psychiatry Fellowship).
2016: The residency program’s existing women’s health curriculum is expanded and becomes a formalized Women’s Mental Health Area of Concentration (now known as the Reproductive Psychiatry and Women’s Mental Health Area of Concentration).

2018: The Department of Psychiatry establishes the innovative Psychiatry Boot Camp, enabling MS4 medical students to work on core psychiatry knowledge and skills just prior to the transition to residency.
Early-Career Clinician-Educator Faculty Members
2011: The Department establishes the Clinician-Educator Faculty Development Program (CEFDP) to support the academic career development of physicians.
2016: The Clinician-Educator Navigator Program matches each new physician with a point person who provides valuable guidance and resources.
Clinician-Educators
2012: The Department holds its first annual Clinician-Educator Showcase, which highlights clinical and educational innovations as well as quality improvement programs.
2017: The Clinical Value Project (CVP) Program funds projects designed to increase the quality of patient care, patient engagement and satisfaction, clinical outcomes, access to services, and clinician efficiency and satisfaction.
Developing Independent Investigators
2010: Launch of the Second Year Faculty Consultation, guiding K awardees and early-career faculty in planning for research independence through structured reflection and senior faculty mentorship.
 2011: The revised and expanded “K Concept Review” supports investigators during the development of National Institutes of Health (NIH) K award grant proposals.
2011: The revised and expanded “K Concept Review” supports investigators during the development of National Institutes of Health (NIH) K award grant proposals. 2017: The Department institutes the First Independent Research Support & Transition (FIRST) Process, helping early-career faculty submit competitive R-series award applications. In addition, the PRIME-the-R Program was introduced as a funding mechanism to support junior faculty preparing their first R-series grant.
Emerging Clinical and Research Focus Areas
2020: Our long-standing telepsychiatry program was expanded to include TeleED which provides psychiatric consultations to Emergency Departments throughout the UPMC hospital system.
2021: The REACH Collaborative supports faculty and trainees in developing community-engaged research projects that address structural drivers of mental health disparities. Through mentorship, resource sharing, and collaborative partnerships, REACH fosters a culture of equity-focused inquiry across the Department.
2023-2024: A group of expert faculty members collaborate to advance research and clinical care in interventional psychiatry. The Department holds the first annual Interventional Psychiatry Showcase, and establishes the Concentration in Interventional Psychiatry, which provides hands-on training in this emerging field to psychiatry residents.
2025: The Digital Mental Health Program connects over 20 faculty members exploring novel technologies to detect, manage, and treat mental health conditions. Through consultation and training in areas such as passive sensing, machine learning, just-in-time interventions, wearables, social media, and large language models, the program fosters innovation in technology-enhanced mental health care.
