Hot Publication - D'Aiuto et al. in the Schizophrenia Bulletin
Persistent Infection by HSV-1 Is Associated with Changes in Functional Architecture of iPSC-Derived Neurons and Brain Activation Patterns Underlying Working Memory Performance
D'Aiuto L, Prasad KM, Upton CH, Viggiano L, Milosevic J, Raimondi G, McClain L, Chowdari K, Tischfield J, Sheldon M, Moore JC, Yolken RH, Kinchington PR, and Nimgaonkar VL
Schizophrenia Bulletin, 2015, 41(1): 123–132
Herpes simplex virus, type 1 (HSV-1) commonly produces lytic mucosal lesions. Invariably it initiates latent infection in sensory ganglia enabling persistent, lifelong infection. Although acute HSV-1 encephalitis is rare and definitive evidence of latent infection in the brain is lacking, exposure untraceable to encephalitis has been repeatedly associated with impaired working memory and executive functions, particularly among schizophrenia patients.
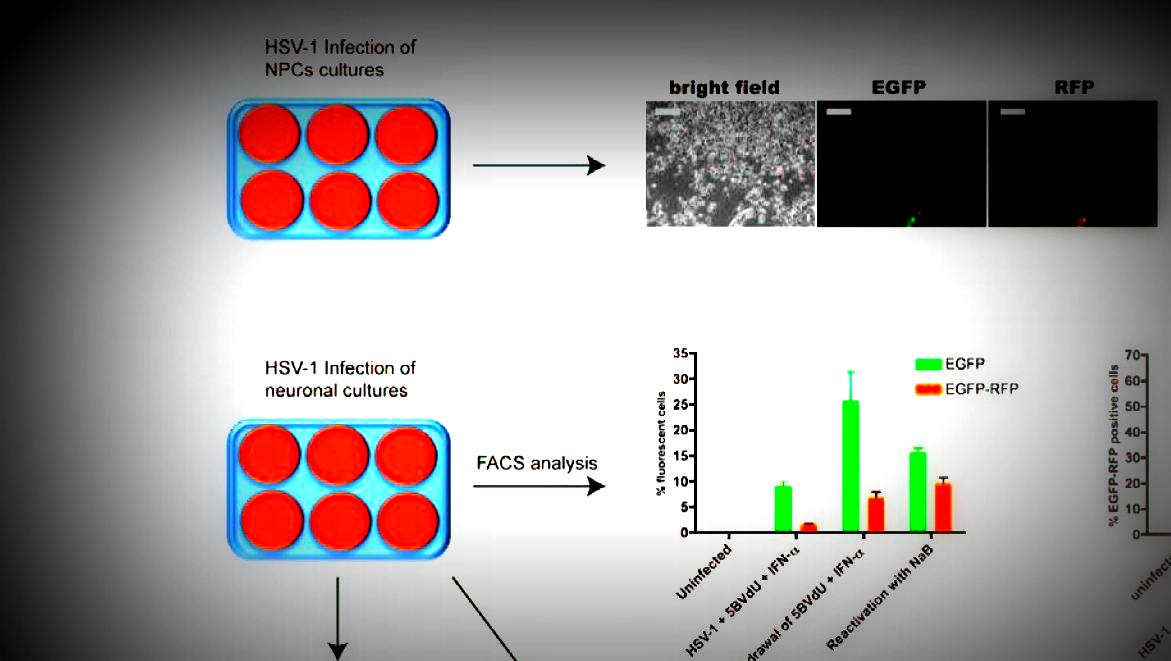
Investigators in the Genetics and Psychosis Program, led by Drs. Leonardo D'Aiuto, Konasale Prasad and Vishwajit Nimgaonkar, examined the patterns of HSV-1 infection and gene expression changes in human induced pluripotent stem cell (iPSC)-derived neurons. Using functional magnetic resonance imaging (fMRI) among schizophrenia cases and controls, the team separately investigated differences in blood oxygenation level-dependent responses to working memory challenges using letter n-back tests.
The researchers found that HSV-1 induced lytic changes in iPSC-derived glutamatergic neurons and neuroprogenitor cells and in neurons, HSV-1 also entered a quiescent state following coincubation with antiviral drugs, with distinctive changes in gene expression related to functions such as glutamatergic signaling. Through their fMRI study, Dr. D'Aiuto and his colleagues also observed the main effects of schizophrenia (P = .001) and HSV-1 exposure (1-back, P = 1.76 × 10- 4; 2-back, P = 1.39 × 10- 5) on blood oxygenation level-dependent responses. They noted increased blood oxygenation level-dependent responses in the frontoparietal, thalamus, and midbrain regions among HSV-1 exposed schizophrenia cases and controls, compared with unexposed persons.
The results of this study are important on multiple levels. First, the lytic/quiescent cycles in iPSC-derived neurons indicate that persistent neuronal infection can occur, altering cellular function. Second, the fMRI studies affirm the associations between nonencephalitic HSV-1 infection and functional brain changes linked with working memory impairment. Together, the fMRI and iPSC studies provide putative mechanisms for the cognitive impairments linked to HSV-1 exposure.
Contributors
Leonardo D'Aiuto, PhD; Konasale M. Prasad, MD; Catherine H. Upton, BA; Lora McClain, BS; Kodavali Chowdari, MD; and Vishwajit L. Nimgaonkar, MD, PhD (Department of Psychiatry, University of Pittsburgh)
Jadranka Milosevic, PhD (Division of Pulmonary, Allergy and Critical Care Medicine, University of Pittsburgh)
Paul R. Kinchington, PhD (Departments of Ophthalmology and Molecular Genetics & Biochemistry, University of Pittsburgh)
Luigi Viggiano, PhD (Department of Biology, University of Bari, Aldo Moro, Bari, Italy)
Giorgio Raimondi, PhD and Robert H. Yolken, MD (Departments of Plastic and Reconstructive Surgery, and Pediatrics, Johns Hopkins University)
Jay Tischfield, PhD; Michael Sheldon, PhD; and Jennifer C. Moore, PhD (Department of Genetics, Rutgers, The State University of New Jersey)
The results of this study were published in the Schizophrenia Bulletin. Click here for a link to the abstract.
