American Journal of Psychiatry: The Nature of Prefrontal Cortical GABA Neuron Alterations in Schizophrenia: Markedly Lower Somatostatin and Parvalbumin Gene Expression Without Missing Neurons
Alterations in markers of cortical gamma-aminobutyric acid (GABA) signaling are among the most widely replicated findings in postmortem brain studies of schizophrenia. In the dorsolateral prefrontal cortex, consistent findings of lower levels of gene products related to GABA neuron signaling indicates that inhibitory neurotransmission signaling is weaker in people with schizophrenia. However, clarity regarding whether these findings reflect lower transcript levels per neuron, fewer neurons, or both, has thus far remained elusive.
Distinguishing among these three alternatives has major implications for understanding the pathogenesis of, and developing novel treatment strategies for, dorsolateral prefrontal cortex dysfunction in schizophrenia. For example, the possibility of missing neurons in the dorsolateral prefrontal cortex in schizophrenia, due to either incomplete neural migration or excessive neuronal death, has inspired interest in transplantation of embryonic GABA neurons as a therapeutic strategy. In contrast, the alternative view (that cortical GABA neurons are present but functionally altered in schizophrenia) has motivated efforts to develop therapeutics that augment the function of the affected GABA neuron subtypes. In addition, the distinction carries important implications for the development of animal models used in the study of schizophrenia, as these model systems should incorporate the nature of GABA neuron alterations observed in the postmortem brains of people with schizophrenia.
However, studies published to date examining GABA signaling in schizophrenia have yielded multiple disparate findings. A major problem in all these studies has been the inability to distinguish between neurons that were missing and neurons that were missed because the single marker used to detect those neurons fell below the level of detectability of the assay used.
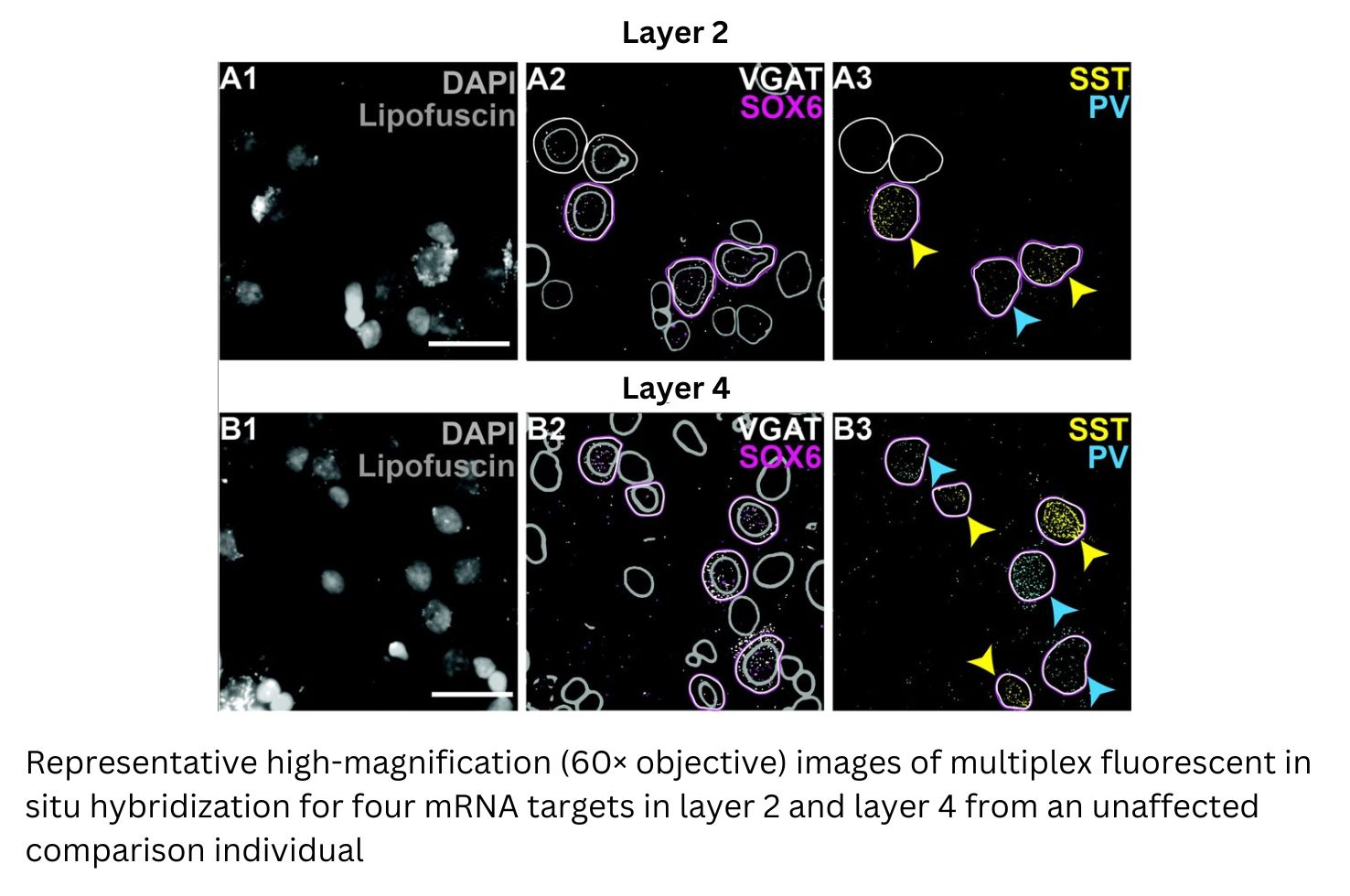
Pitt Psychiatry investigators including Samuel Dienel (Medical Science Training Program student); Kenneth Fish, PhD (Associate Professor of Psychiatry); and David Lewis, MD (Distinguished Professor of Psychiatry and Neuroscience, Thomas Detre Professor of Academic Psychiatry), sought to determine whether the well-documented lower tissue levels of somatostatin and parvalbumin mRNAs in schizophrenia are due to lower levels of these transcripts per neuron, fewer neurons that contain these transcripts, or both. To do so, the scientists used a novel multiplex fluorescent in situ hybridization approach to label four mRNA targets simultaneously with cellular resolution. This approach, which has not previously been used in postmortem human brain studies, permits the independent determination of transcript levels per neuron and of neuron density without conflating the two measures. They focused their analysis on layers 2 and 4 of the human dorsolateral prefrontal cortex, as these layers exhibit the highest density of GABA neurons and are differentially enriched for somatostatin and parvalbumin neurons, respectively.
In a study recently published in The American Journal of Psychiatry, the investigators reported that in schizophrenia, pronounced somatostatin and parvalbumin mRNA deficits are attributable to lower levels of each transcript per neuron, not fewer neurons. Instead of missing, these neurons appear to be functionally altered and thus amenable to therapeutic interventions.
“These findings clearly resolve a long-standing area of confusion in schizophrenia research and provide compelling evidence that refutes two hypotheses about the pathogenesis of the illness: failure of neuronal migration and excessive neuronal death. In addition, the findings demonstrate the potential value of therapeutic strategies that target the functional properties of somatostatin and/or parvalbumin neurons,” said Dr. Lewis, the study’s senior author.
The Nature of Prefrontal Cortical GABA Neuron Alterations in Schizophrenia: Markedly Lower Somatostatin and Parvalbumin Gene Expression Without Missing Neurons
Dienel SJ, Fish KN, Lewis DA.
The American Journal of Psychiatry Published Online:19 Apr 2023 https://doi.org/10.1176/appi.ajp.20220676
